CMS 1500 Claim Form in Healthcare
Strong 8k brings an ultra-HD IPTV experience to your living room and your pocket.
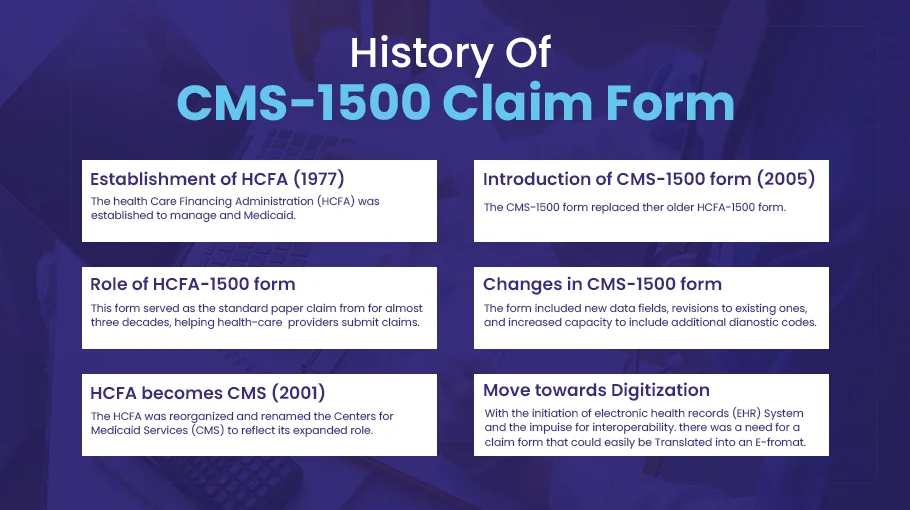
Introduction to CMS 1500 Claim Form
In the intricate world of healthcare billing, the CMS 1500 claim form stands as a fundamental document. This standardized form, recognized by the Centers for Medicare & Medicaid Services (CMS), serves as a vital tool for healthcare providers to bill insurance companies for services rendered to patients. Let's delve into the significance and intricacies of the CMS 1500 claim form in healthcare in the realm of healthcare administration.
Purpose of the CMS 1500 Claim Form
The primary purpose of the CMS 1500 claim form is to facilitate the billing process between healthcare providers and insurance companies. It serves as a comprehensive record of the services provided to patients, including medical procedures, treatments, and diagnostic tests. By accurately documenting these services, the form enables providers to request reimbursement from insurance carriers effectively.
Components of the CMS 1500 Claim Form
The CMS 1500 claim form consists of various sections, each designed to capture specific details about the patient, the provider, and the services rendered. From patient demographics to diagnosis codes, every field plays a crucial role in ensuring accurate billing and reimbursement.
Completing the CMS 1500 Claim Form
Filling out the CMS 1500 claim form requires meticulous attention to detail to avoid errors and delays in payment. Healthcare providers must accurately enter patient information, procedure codes, and diagnosis codes, following standardized guidelines to ensure compliance with insurance regulations.
Importance of Accuracy
Accuracy is paramount when completing the CMS 1500 claim form. Even minor errors or omissions can lead to claim denials, delayed payments, or audits. By maintaining accuracy and integrity in the billing process, healthcare providers can minimize financial losses and maintain regulatory compliance.
Submission and Processing
Once the CMS 1500 claim form is completed, it is submitted to the appropriate insurance carrier for processing. The form undergoes rigorous scrutiny to verify the accuracy of the information provided before reimbursement is issued to the healthcare provider.
CMS 1500 Claim Form and Electronic Health Records (EHR)
With the advent of electronic health records (EHR) systems, the process of submitting CMS 1500 claim forms has become more streamlined and efficient. Integration with EHR platforms allows for seamless transfer of patient data, reducing the risk of errors and expediting the billing process.
Reimbursement and Payment
Reimbursement rates for services rendered are determined by various factors, including the type of insurance coverage and contractual agreements between providers and payers. Once a claim is approved, payment is typically issued within a specified timeframe, ensuring timely compensation for healthcare services.
Compliance and Regulations
Adherence to regulatory guidelines, such as those outlined by the Health Insurance Portability and Accountability Act (HIPAA), is essential when handling sensitive patient information on the CMS 1500 claim form. Healthcare providers must maintain strict compliance with data privacy and security standards to safeguard patient confidentiality and avoid legal repercussions.
Common Challenges and Solutions
Navigating the complexities of the CMS 1500 claim form can pose challenges for healthcare providers, from deciphering coding guidelines to resolving claim denials. Implementing robust training programs and utilizing electronic billing software can help address common issues and improve overall efficiency in the billing process.
Future of CMS 1500 Claim Form
As technology continues to evolve, so too will the CMS 1500 claim form. From electronic submission enhancements to updates in coding standards, ongoing innovations will shape the future of healthcare billing, driving greater efficiency and accuracy in claims processing.
Training and Education
To ensure proficiency in handling CMS 1500 claim forms, healthcare providers must invest in comprehensive training and education for administrative staff. By equipping personnel with the necessary skills and knowledge, providers can optimize the billing process and minimize errors.
Case Studies and Examples
Real-life case studies provide valuable insights into successful claim submissions and highlight best practices for navigating the CMS 1500 claim form. By studying these examples, healthcare providers can gain practical knowledge and apply proven strategies to improve their billing workflows.
FAQs about CMS 1500 Claim Form
1. What is the CMS 1500 claim form used for?
The CMS 1500 claim form is used by healthcare providers to bill insurance companies for services rendered to patients.
2. What are the key components of the CMS 1500 claim form?
The form includes fields for patient demographics, provider information, diagnosis codes, and procedure codes, among other details.
3. How important is accuracy when completing the CMS 1500 claim form?
Accuracy is crucial to avoid claim denials, delayed payments, and compliance issues with insurance regulations.
4. How does electronic health records (EHR) integration impact the billing process?
EHR integration streamlines the submission of CMS 1500 claim forms, reducing errors and expediting reimbursement.
5. What are some common challenges healthcare providers face when completing CMS 1500 claim forms?
Common challenges include deciphering coding guidelines, resolving claim denials, and maintaining compliance with regulatory standards.
Note: IndiBlogHub features both user-submitted and editorial content. We do not verify third-party contributions. Read our Disclaimer and Privacy Policyfor details.