Nano-Based in Situ Cancer Vaccine

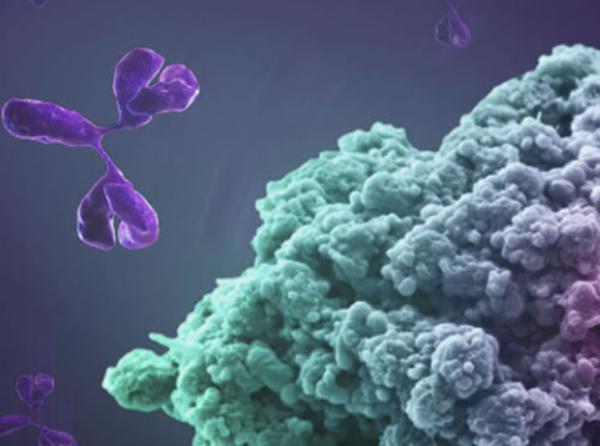
Cancer immunotherapy has shown great promise in cancer treatment over the last decade. Several cancer immunotherapies, such as immune checkpoint blockade therapies, cancer vaccines, and CAR-T therapies, have been extensively researched and have yielded promising results.
Cancer vaccines, which elicit tumor-specific immune stimulation, are one of the most important immunotherapeutic strategies and have great potential in cancer treatment. Patients have responded favorably to cancer vaccines based on neoantigens and messenger RNA (mRNA).
Despite enormous efforts in the development of cancer vaccines, which are still in the cancer prevention phase, eliciting a large number of immune responses in cancer patients remains a significant challenge, owing to the cancer vaccines' low immunogenicity, the immunosuppressive tumor microenvironment, and the ground correlation between antigens in cancer vaccines and specific patient tumors.
Autologous tumors have been used to produce cancer vaccines in vitro or in vivo, so-called personalized cancer vaccines, to improve the therapeutic efficacy of cancer vaccines. Autologous tumor cell-based cancer vaccines benefit from tumor-specific tumor-associated antigens (TAA) and induce a stronger immune response than conventional cancer vaccines.
However, in vitro preparation of autologous tumor cell cancer vaccines suffers from complex processes, low yields, and suboptimal efficacy, which limit the clinical application of autologous tumor vaccines. In contrast, large-scale in situ generation of autologous tumor cell cancer vaccines in vivo avoids the complex in vitro vaccine preparation process and is ideal for the production of cancer vaccines.
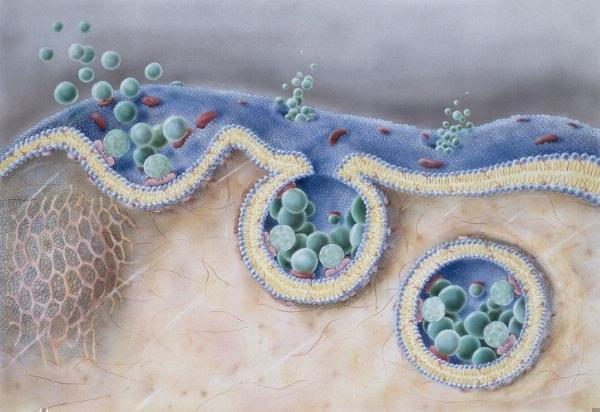
On November 1, 2022, Fu-Gen Wu's team from Southeast University's School of Bioscience and Medical Engineering published a research paper in Nature Communications titled: In situ generation of micrometer-sized tumor cell-derived vesicles as autologous cancer vaccines for boosting systemic immune responses. HDDT nanoparticles were created using dendritic polymers loaded with adriamycin (DOX), tyrosine kinase inhibitor (TKI), and hyaluronic acid (HA) encapsulated nanoparticles. HDDT nanoparticles have the ability to convert 100% of cancer cells into micron-sized vesicles (HMVs).
Experiments in tumor mouse models revealed that HDDT nanoparticles could inhibit tumor growth, induce strong immunogenic cell death, and convert primary tumors into antigenic reservoirs by producing HMVs in situ as personalized cancer vaccines for cancer immunotherapy. Furthermore, after HDDT nanoparticle treatment, tumor model mice showed strong immune memory effects, which could prevent tumor recurrence in the long run.
In this study, the research team fabricated a series of nanobombs (NBs), including dendritic polymers (Dendritic Polymers) loaded with adriamycin (DOX, an anti-cancer drug) and tyrosine kinase inhibitors (TKI, an anti-cancer drug) and hyaluronic acid (HA, used for tumor targeting) encapsulation, called HDDT NBs.
The team found that after treatment of cancer cells with HDDT NBs, almost all cells (10-30 microns in diameter) were transformed into uniform micron-sized vesicles (1.6-3.2 microns), and cell-to-vesicle conversion efficiency was as high as 100%, meaning that all cancer cells could be efficiently converted into HDDT-induced micron-sized vesicles (HMVs).
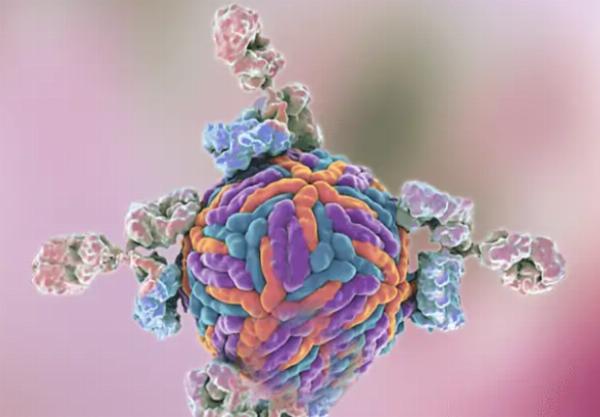
Further studies revealed that HDDT NBs, after systemic administration, could accumulate in tumor areas, inhibit tumor growth under different tumor models, induce immunogenic cell death on a large scale, and produce HMVs in situ, transforming tumor tissues into antigenic reservoirs. Immune checkpoint blockade therapy, alone or in combination, could induce intra-tumor and systemic immune responses, establish a strong immune memory effect, cure mouse tumors, and effectively protect against recurrence.
Overall, the HDDT-induced micron-sized vesicles (HMVs) developed in this study provide a simple and promising nanotechnology-based strategy for the in situ production of autologous tumor cell vaccines and may provide clues for the development of personalized cancer vaccines.https://www.creative-biolabs.com/vaccine/cancer-vaccines.htm
Note: IndiBlogHub features both user-submitted and editorial content. We do not verify third-party contributions. Read our Disclaimer and Privacy Policyfor details.