Pain and Mental Well-Being: Examining the Mutual Association
Strong 8k brings an ultra-HD IPTV experience to your living room and your pocket.
First of all,
Pain and mental health have a complicated, reciprocal relationship in which each has a big impact on the other. Mental health issues can affect how people perceive and cope with pain, and they can also increase vulnerability to it. Anxiety, depression, and post-traumatic stress disorder (PTSD) are just a few of the conditions that chronic pain can lead to or exacerbate. Comprehending the interdependent connection between psychological well-being and pain is crucial for optimizing healthcare administration and enhancing general health. In addition to examining common symptoms and issues, this article addresses the reciprocal relationship between pain and mental health and offers techniques for resolving both.
The Mutual Association Between Pain and Mental Well-Being:
There are several physiological, psychological, and social factors that link pain and mental health. The following are some crucial elements of the reciprocal relationship between pain and mental health:
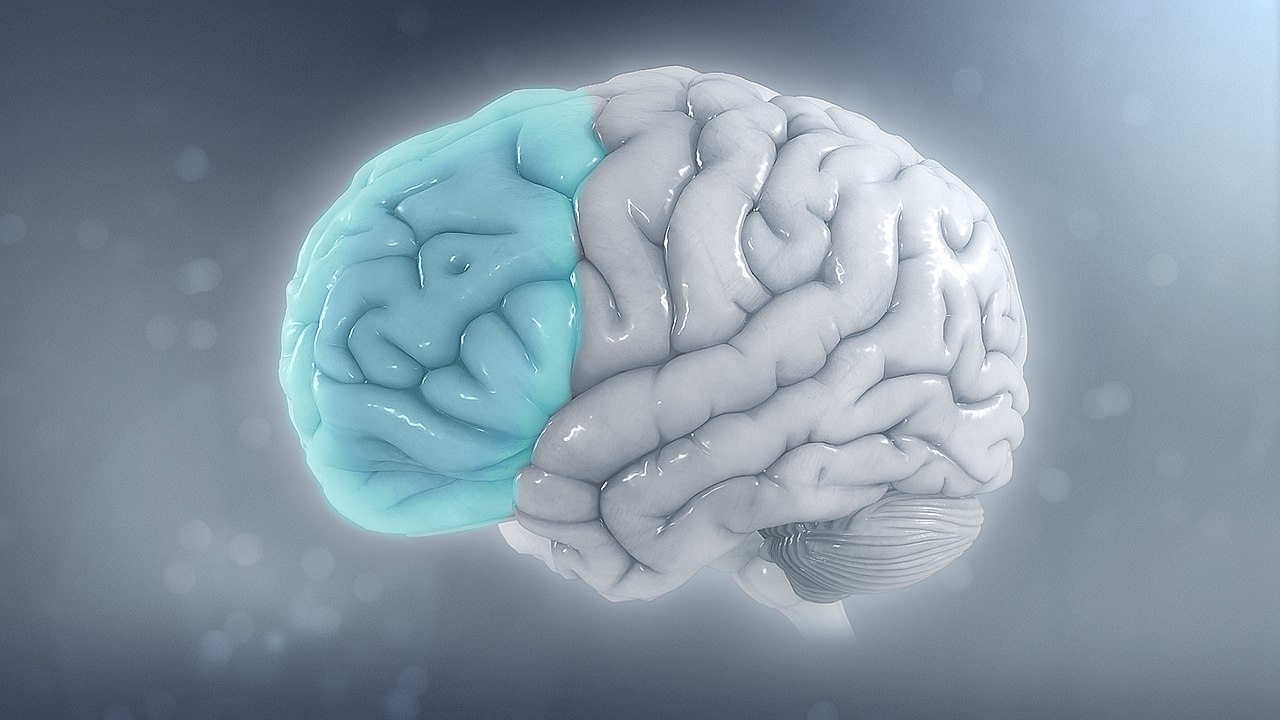
Physiological Mechanisms:
Changes in neurotransmitter levels, neuroendocrine dysfunction, and dysregulation of the hypothalamic-pituitary-adrenal (HPA) axis are among the neurobiological routes and mechanisms that chronic pain and mental health disorders have in common. Pain and mental health symptoms can both arise or worsen as a result of these physiological alterations.
Psychological Factors:
Stress, anxiety, and negative affect are examples of psychological factors that can intensify pain perception and play a role in the emergence of chronic pain syndromes. On the other hand, psychological distress brought on by persistent pain, such as hopelessness, frustration, and a loss of control, can aggravate mental health conditions and weaken coping skills.
Behavioral Reactions:
Mental health conditions and chronic pain can affect people's coping mechanisms and behavioral reactions. Avoidant behaviors, social disengagement, or substance abuse are examples of maladaptive coping strategies used by people to deal with pain or ease psychological suffering. These actions may worsen an existing pain and mental health symptom loop, making impairment and disability more severe.
Social Impact:
People's experiences and results might be influenced by the social context in which mental health illnesses and pain arise. The ability of individuals to manage pain and mental health issues, as well as to obtain appropriate therapy and resources, can be influenced by various factors such as social support, socioeconomic level, healthcare accessibility, and cultural norms.
Typical Signs and Difficulties:
Pain and mental health sufferers may experience a variety of symptoms and difficulties, such as:
Chronic Pain:
Pain that is continuous or recurrent and lasts longer than anticipated—often months or years—is referred to as chronic pain. Fibromyalgia, low back pain, migraines, neuropathic pain, and musculoskeletal problems are among the common causes causing chronic pain. Chronic pain can have a major negative influence on mobility, quality of life, and day-to-day functioning. This can result in disability, lower productivity, and social isolation.
Anxiety Disorders:
Excessive concern, fear, or trepidation about circumstances or occurrences in the future are symptoms of anxiety disorders. Panic disorder, social anxiety disorder, generalized anxiety disorder (GAD), and particular phobias are examples of common anxiety disorders. Excessive vigilance, rumination, and tense muscles are examples of anxiety symptoms that can amplify pain perception and disrupt pain management techniques.
Depression:
Prolonged melancholy, hopelessness, and a loss of interest in or enjoyment from activities are symptoms of depression. Physical symptoms of depression might include exhaustion, changes in weight or appetite, and trouble sleeping. Suicide and disability risk are raised, pain symptoms can get worse, and functioning can be compromised by depression.
A stressful occurrence, such as a catastrophic injury, accident, or attack, might cause someone to experience post-traumatic stress disorder (PTSD). Hypervigilance, avoiding reminders of the event, intrusive memories or flashbacks, and emotional numbness are some of the symptoms of post-traumatic stress disorder (PTSD). PTSD can worsen pain sensations, make a person more sensitive to pain, and obstruct attempts at healing and rehabilitation.
Handling Issues Related to Pain and Mental Health:
It takes a thorough, interdisciplinary approach that takes into account physiological, psychological, and social elements to address both pain and mental health issues. Among the methods for dealing with pain and mental health issues are:
Integrated Treatment Approaches:
For those with co-occurring pain and mental health issues, combining pain management and mental health care into a unified care plan can help improve outcomes. Coordination between medical professionals, such as doctors, psychologists, physical therapists, and social workers, is a key component of collaborative care models that offer comprehensive assistance and address the psychological and physical components of pain and mental health issues.
Psychotherapy:
Psychotherapy, including mindfulness-based therapies, cognitive-behavioral therapy (CBT), and acceptance and commitment therapy (ACT), can assist people in managing pain-related distress, coping skill development, and addressing maladaptive thoughts and behaviors related to pain and mental health disorders. In addition, psychotherapy can help people become more resilient, better at controlling their emotions, and feel better overall.
Medication Management:
To treat pain and symptoms related to mental health, doctors may prescribe pharmacological therapies such as anxiolytics, antidepressants, and anticonvulsants. Optimizing treatment outcomes and limiting risks need careful medication management, which includes monitoring for possible side effects and drug interactions.
Pain Rehabilitation Programs:
Individuals with chronic pain and mental health comorbidities can benefit from comprehensive, evidence-based interventions provided by multidisciplinary pain rehabilitation programs. To relieve pain, increase functionality, and improve quality of life, these programs usually combine medical management with physical therapy, occupational therapy, behavioral therapy, and education.
Self-Management Techniques:
Using self-management techniques to enable people to take an active role in their own care can boost results and self-efficacy. Promoting self-care practices like exercise, mindfulness, stress reduction, and healthful living can help people cope with pain and mental health issues more effectively and enhance their general well-being.
In summary:
The importance of addressing both the physical and psychological parts of people's experiences is highlighted by the reciprocal relationship that exists between pain and mental health. Both mental health issues and chronic pain frequently coexist and have a substantial negative influence on a person's functioning, quality of life, and general well-being. Healthcare professionals may effectively treat and support patients with pain and mental health issues by using a thorough, interdisciplinary approach that takes into account physiological, psychological, and social variables. Giving people the tools they need to take an active role in their own treatment, building resilience, and encouraging self-management techniques can all help people function better, manage pain and mental health issues more effectively, and live better overall.
Note: IndiBlogHub features both user-submitted and editorial content. We do not verify third-party contributions. Read our Disclaimer and Privacy Policyfor details.







