A Step-by-Step Guide to Liver Cirrhosis Treatment
Strong 8k brings an ultra-HD IPTV experience to your living room and your pocket.
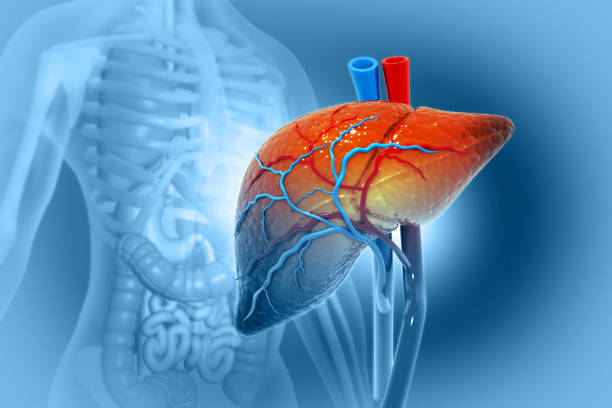
Liver cirrhosis is a progressive condition where healthy liver tissue is replaced by scar tissue, impairing the liver’s ability to function. It is often the result of chronic liver damage caused by factors such as alcohol abuse, hepatitis, fatty liver disease, or certain inherited conditions. While cirrhosis cannot be reversed, its progression can be managed, and symptoms can be alleviated with appropriate treatment. This guide outlines the steps involved in treating Liver Cirrhosis Treatment in Dubai, focusing on lifestyle changes, medications, and advanced treatments to slow disease progression and improve overall quality of life.
Step 1: Diagnosis and Evaluation
The first step in managing liver cirrhosis is an accurate diagnosis and understanding of the disease’s progression. This is typically done through a combination of medical history, physical examination, and diagnostic tests.
Medical History and Physical Examination
Your doctor will ask about your symptoms, medical history, lifestyle habits, and risk factors for liver disease, such as heavy alcohol use, a history of viral hepatitis, obesity, or family history of liver conditions. During the physical examination, signs of cirrhosis may be evident, such as jaundice (yellowing of the skin), an enlarged liver or spleen, fluid retention, or swollen veins.
Diagnostic Tests
Once cirrhosis is suspected, the following tests will help confirm the diagnosis and assess the extent of liver damage:
Blood Tests: These tests measure liver enzymes, bilirubin levels, albumin, and clotting factors to assess liver function.
Imaging Studies: Ultrasound, CT scans, or MRI may be used to examine the liver’s size, structure, and any complications like varices or ascites.
Liver Biopsy: A biopsy is a definitive test that involves taking a sample of liver tissue to evaluate the extent of scarring.
FibroScan (Elastography): This non-invasive test measures liver stiffness, which correlates with the degree of fibrosis or cirrhosis.
Step 2: Treating the Underlying Cause
Once cirrhosis is diagnosed, treating the underlying cause is essential to slow down or prevent further liver damage. The treatment plan will vary based on the cause of cirrhosis.
1. Alcohol-Related Cirrhosis
If cirrhosis is caused by chronic alcohol use, complete abstinence from alcohol is the most important first step in treatment. Continued drinking will accelerate liver damage and worsen cirrhosis. To manage alcohol dependence, therapy, counseling, and support groups such as Alcoholics Anonymous (AA) can be beneficial. In some cases, medications like disulfiram or acamprosate may be prescribed to help manage alcohol cravings.
2. Chronic Hepatitis B or C
If hepatitis B or C is the underlying cause of cirrhosis, antiviral treatment is needed to suppress the virus and prevent further liver damage.
Hepatitis B: Antiviral medications like tenofovir or entecavir are used to suppress the virus, but they typically need to be taken for a long period.
Hepatitis C: The introduction of direct-acting antivirals (DAAs) has revolutionized hepatitis C treatment. DAAs, such as sofosbuvir and ledipasvir, can cure hepatitis C in most patients, thus preventing cirrhosis progression.
3. Nonalcoholic Fatty Liver Disease (NAFLD) / Nonalcoholic Steatohepatitis (NASH)
For NAFLD or NASH, lifestyle modifications are the cornerstone of treatment. Key steps include:
Weight loss: Gradual weight loss (5-10% of body weight) can significantly reduce liver fat, inflammation, and scarring.
Dietary changes: A balanced diet, such as the Mediterranean diet, helps improve liver health. This includes eating more fruits, vegetables, whole grains, healthy fats, and lean protein while avoiding processed foods and sugars.
Exercise: Regular physical activity helps reduce fat buildup in the liver and can improve insulin sensitivity.
Medications for NASH are still under investigation, but pioglitazone (a diabetes medication) and Vitamin E have shown some benefits in reducing liver inflammation.
4. Autoimmune Hepatitis
If cirrhosis is caused by autoimmune hepatitis, immunosuppressive medications such as corticosteroids (e.g., prednisone) and azathioprine are commonly used to reduce inflammation and prevent further liver damage.
5. Genetic Disorders
For cirrhosis caused by genetic disorders, such as hemochromatosis (iron overload) or Wilson’s disease (copper buildup), specific treatments include:
Phlebotomy for hemochromatosis to remove excess iron from the blood.
Chelating agents, such as penicillamine or trientine, are used to remove excess copper in Wilson’s disease.
Step 3: Symptom Management and Preventing Complications
As cirrhosis progresses, managing symptoms and preventing complications becomes essential. Depending on the severity of the disease, medications and interventions are required to alleviate symptoms.
1. Managing Ascites (Fluid Retention)
Ascites is the accumulation of fluid in the abdomen, which is common in advanced cirrhosis. To manage ascites:
Diuretics like spironolactone and furosemide are used to remove excess fluid from the body.
Paracentesis, a procedure in which a needle is used to drain excess fluid, may be performed if ascites becomes severe.
2. Preventing Variceal Bleeding
Cirrhosis can lead to portal hypertension, increasing pressure in the veins of the esophagus and stomach, which can cause varices (swollen veins) to rupture and bleed. To prevent bleeding:
Beta-blockers, such as propranolol, are often prescribed to reduce portal pressure.
Endoscopic therapy (band ligation or sclerotherapy) may be used to treat bleeding varices.
3. Treating Hepatic Encephalopathy
Hepatic encephalopathy is a condition in which toxins build up in the brain due to impaired liver function, causing confusion, altered mental state, and other neurological symptoms. Treatment includes:
Lactulose, a medication that reduces toxin absorption and helps with bowel movements.
Rifaximin, an antibiotic that reduces ammonia-producing bacteria in the intestines.
4. Managing Jaundice and Itching
Jaundice (yellowing of the skin and eyes) occurs when the liver is unable to process bilirubin effectively. Treatment options may include:
Medications such as ursodeoxycholic acid to help reduce bilirubin levels.
Antihistamines to manage itching (pruritus), a common symptom of cirrhosis.
Step 4: Advanced Treatments for Severe Cirrhosis
In cases where cirrhosis has reached an advanced stage, more intensive interventions may be needed.
1. Liver Transplantation
For patients with end-stage cirrhosis, a liver transplant may be necessary. This procedure involves replacing the diseased liver with a healthy liver from a donor. The decision to pursue a transplant is typically based on the Model for End-Stage Liver Disease (MELD) score, which assesses liver function and helps determine transplant eligibility. A successful transplant can significantly improve a patient's life expectancy and quality of life, but lifelong immunosuppressive medications are required to prevent rejection.
2. Transjugular Intrahepatic Portosystemic Shunt (TIPS)
In some cases of portal hypertension, when variceal bleeding or ascites is not manageable by other means, TIPS may be recommended. This procedure creates a shunt between the liver and the veins to reduce portal pressure and alleviate complications.
Step 5: Ongoing Monitoring and Long-Term Care
Cirrhosis is a chronic condition that requires ongoing care and monitoring. Regular check-ups are essential to:
Monitor liver function through blood tests and imaging studies.
Screen for liver cancer (hepatocellular carcinoma), especially in patients with chronic hepatitis or cirrhosis.
Assess for complications such as varices, ascites, or hepatic encephalopathy.
Ensure adherence to prescribed treatments and medications.
Adopting a liver-friendly lifestyle is critical. This includes maintaining a healthy weight, following a balanced diet, avoiding alcohol and hepatotoxic substances, and managing other conditions such as diabetes, hypertension, and high cholesterol.
Conclusion
Liver cirrhosis is a serious condition, but with early diagnosis, effective treatment, and ongoing care, its progression can be slowed, and complications can be managed. The treatment plan for cirrhosis will vary depending on the cause of the disease, its severity, and the presence of complications. Key aspects of treatment include addressing the underlying cause, managing symptoms, preventing complications, and, in some cases, undergoing advanced treatments like liver transplantation. With proper management, people with cirrhosis can lead fulfilling lives and significantly improve their overall health.
Note: IndiBlogHub features both user-submitted and editorial content. We do not verify third-party contributions. Read our Disclaimer and Privacy Policyfor details.


