SVT Unmasked: A Deep Dive into ECG Patterns and Diagnosis

Strong 8k brings an ultra-HD IPTV experience to your living room and your pocket.
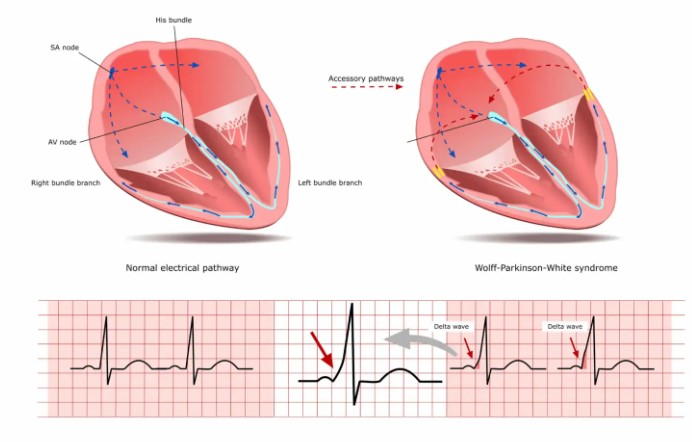
Supraventricular tachycardia (SVT) is a common cardiac arrhythmia characterized by rapid heartbeats originating above the ventricles. In this blog, we delve into the intricacies of SVT, exploring its clinical significance, ECG manifestations, diagnostic criteria, and management strategies.
1. Understanding Supraventricular Tachycardia
SVT encompasses a group of arrhythmias originating from the atria or the atrioventricular node, leading to abnormally fast heart rates exceeding 100 beats per minute. This condition can manifest as sudden palpitations, chest discomfort, dizziness, and shortness of breath, significantly impacting an individual's quality of life. While SVT episodes are often paroxysmal and self-limiting, they can occasionally result in hemodynamic compromise and necessitate prompt medical intervention.
2. Electrocardiogram (ECG) Features
ECG analysis plays a pivotal role in diagnosing SVT and differentiating it from other types of tachyarrhythmias. Key ECG features suggestive of SVT include:
- Narrow QRS Complex: SVT typically presents with a narrow QRS complex (
- Regular Rhythm: SVT demonstrates a regular rhythm, with consistent R-R intervals on the ECG tracing.
- Absence of P Waves: In certain SVT subtypes such as atrioventricular nodal reentrant tachycardia (AVNRT) and atrioventricular reentrant tachycardia (AVRT), P waves may be obscured or buried within the QRS complex, leading to the appearance of absent or retrograde P waves.
- ST-T Changes: Transient ST segment deviations and T wave abnormalities may occur during SVT episodes, reflecting myocardial ischemia or altered ventricular repolarization secondary to rapid heart rates.
3. Diagnostic Criteria
Differentiating various forms of supraventricular tachycardia ecg requires a systematic approach and adherence to specific diagnostic criteria. While the presence of a narrow QRS complex and regular rhythm are hallmark features of SVT, additional ECG findings such as P wave morphology, PR interval duration, and QRS morphology aid in subtype classification. Clinicians utilize electrophysiological studies (EPS) and pharmacological maneuvers such as adenosine administration to further characterize and confirm the diagnosis of SVT and identify potential therapeutic targets.
4. Differential Diagnosis
Distinguishing SVT from other tachyarrhythmias, such as ventricular tachycardia (VT) and atrial fibrillation (AF), is essential for guiding appropriate management strategies. VT typically presents with wide QRS complexes (> 0.12 seconds) and irregular rhythms, whereas AF is characterized by rapid, irregular atrial activity without discernible P waves. Careful ECG interpretation, clinical correlation, and consideration of patient history aid in accurate diagnosis and treatment planning.
5. Treatment Modalities
The management of SVT encompasses various therapeutic modalities aimed at terminating acute episodes, preventing recurrences, and reducing long-term cardiovascular risks. Acute termination of SVT often involves vagal maneuvers, such as the Valsalva maneuver or carotid sinus massage, followed by intravenous administration of adenosine or calcium channel blockers. Long-term management may entail pharmacological therapy with antiarrhythmic agents, catheter-based ablation procedures, or implantation of cardiac devices such as pacemakers or implantable cardioverter-defibrillators (ICDs) in select cases.
6. Prognosis and Follow-up
With appropriate diagnosis and management, the prognosis for individuals with SVT is generally favorable. However, recurrent episodes and underlying cardiovascular comorbidities may necessitate regular follow-up evaluations to assess treatment efficacy, monitor for complications, and optimize therapeutic regimens. Lifestyle modifications, including stress reduction, avoidance of triggers, and adherence to medication, play integral roles in long-term arrhythmia management and cardiovascular health maintenance.
Conclusion
Supraventricular tachycardia represents a complex arrhythmic disorder with diverse clinical presentations and management considerations. Through supraventricular tachycardia ecg analysis, adherence to diagnostic criteria, and multidisciplinary collaboration, clinicians can effectively diagnose SVT, tailor appropriate treatment strategies, and optimize patient outcomes. Continued research efforts aimed at elucidating the pathophysiology of SVT and refining therapeutic approaches hold promise for further enhancing the management and prognosis of this prevalent cardiac arrhythmia.
Note: IndiBlogHub features both user-submitted and editorial content. We do not verify third-party contributions. Read our Disclaimer and Privacy Policyfor details.