Understanding Alpha and Beta Emitters in Radiopharmaceuticals
Strong 8k brings an ultra-HD IPTV experience to your living room and your pocket.
Introduction
Radiopharmaceuticals are a cornerstone of modern nuclear medicine, combining radioactive isotopes with pharmaceutical compounds to diagnose and treat various diseases, especially cancer. Among the radioactive components used, alpha and beta emitters stand out due to their distinct radiation properties and therapeutic potentials. Understanding these emitters, their benefits, challenges, and future trends is critical for advancing nuclear medicine and improving patient outcomes.
Definition
Alpha and beta emitters-based radiopharmaceuticals are specialized compounds that contain radioactive isotopes emitting alpha or beta particles, used primarily in targeted cancer therapy. These emitters deliver high-energy radiation directly to diseased tissues, such as tumors, while minimizing damage to surrounding healthy cells. Alpha emitters release heavy, high-energy particles with short penetration ranges, ideal for destroying single cells or small clusters, while beta emitters release lighter particles with deeper tissue penetration, suitable for larger tumors. These radiopharmaceuticals offer precise, localized treatment in nuclear medicine.
What Are Alpha and Beta Emitters?
Delivering targeted radiation to sick cells while preserving healthy tissue is the fundamental idea behind radiopharmaceutical therapy. The radioactive isotopes used in this context emit particles that cause cellular damage, leading to cancer cell death.
Alpha Emitters: Alpha particles are heavy, positively charged particles composed of two protons and two neutrons. They possess high linear energy transfer (LET), meaning they release a large amount of energy over a very short distance, typically a few cell diameters (50-100 micrometers). This high energy density causes significant double-strand DNA breaks, which are lethal to cells.
Beta Emitters: Beta particles are high-energy, high-speed electrons or positrons emitted by certain radioactive nuclei. Beta particles have a lower LET compared to alpha particles and travel farther through tissues (up to several millimeters). They cause cellular damage mainly through ionization and generation of free radicals.
Both types of emitters have unique characteristics that make them suitable for different therapeutic applications.
Benefits of Alpha and Beta Emitters in Radiopharmaceuticals
Benefits of Alpha Emitters
High Potency and Precision: Because alpha particles deposit a large amount of energy within a tiny radius, they can effectively kill cancer cells while minimizing damage to surrounding healthy tissue. This precision is especially advantageous for treating micrometastases and small clusters of cancer cells.
Overcoming Resistance: Some tumors resistant to chemotherapy or beta radiation respond well to alpha therapy due to the irreparable DNA damage alpha particles cause.
Reduced Side Effects: The short path length of alpha particles limits collateral damage, potentially reducing side effects compared to other radiation therapies.
Benefits of Beta Emitters
Suitable for Larger Tumors: Due to their longer tissue penetration, beta emitters are effective for treating larger tumors or more diffuse disease areas where radiation needs to cover more volume.
Established Clinical Use: Beta emitters, like Lutetium-177 and Yttrium-90, have a longer history of clinical use and proven efficacy in various cancers, including neuroendocrine tumors and lymphoma.
Versatile Applications: Beta emitters can be used for both therapy and imaging (when combined with gamma emissions), facilitating treatment planning and monitoring.
Challenges of Using Alpha and Beta Emitters in Radiopharmaceuticals
Challenges with Alpha Emitters
Production and Availability: Alpha emitters like Actinium-225 or Radium-223 are difficult and costly to produce in large quantities. Their limited availability restricts widespread clinical use.
Radiopharmaceutical Development: Creating stable, targeted alpha-emitting radiopharmaceuticals requires sophisticated chemistry to attach alpha emitters to molecules that can selectively target cancer cells without premature release.
Safety Concerns: Despite their short range, alpha emitters are highly radiotoxic if they accumulate in non-target organs. Strict handling and dosage guidelines are required to protect both patients and employees.
Challenges with Beta Emitters
Collateral Damage: Beta particles’ longer tissue penetration increases the risk of damaging healthy tissue surrounding tumors, potentially leading to side effects such as bone marrow suppression.
Radiation Dosimetry: Precise dosimetry is essential to balance effective tumor irradiation with minimizing toxicity, but individual patient variability complicates this process.
Resistance and Relapse: Some tumors may develop resistance to beta radiation or have insufficient uptake of beta-emitting radiopharmaceuticals, reducing treatment effectiveness.
Future Trends in Alpha and Beta Radiopharmaceuticals
The field of radiopharmaceutical therapy is rapidly evolving, driven by technological advances, new isotope production methods, and improved targeting strategies.
Enhanced Targeting and Delivery:
Researchers are developing novel targeting molecules such as peptides, antibodies, and small molecules that can deliver alpha and beta emitters more selectively to tumor cells. These advances aim to improve efficacy and reduce side effects.
Combination Therapies:
Combining alpha and beta emitters with chemotherapy, immunotherapy, or external beam radiation is showing promise. Such combinations may overcome tumor resistance, enhance immune responses, and provide synergistic effects.
New Isotope Production Technologies:
Innovations in isotope production, including accelerator-based methods and improved nuclear reactors, are helping increase the availability of alpha emitters like Actinium-225. This growth will enable broader clinical trials and eventual standard-of-care use.
Personalized Dosimetry and Imaging:
Improved imaging techniques and computational models allow for more personalized dosimetry — tailoring doses to individual patient anatomy and tumor characteristics. Theranostic pairs, where one isotope is used for imaging and another for therapy, enable real-time treatment monitoring and adjustments.
Expanding Indications:
While current approvals focus mainly on specific cancers (e.g., prostate cancer with Radium-223), ongoing research is exploring alpha and beta emitter applications in other solid tumors, hematologic malignancies, and even non-oncological diseases such as infections.
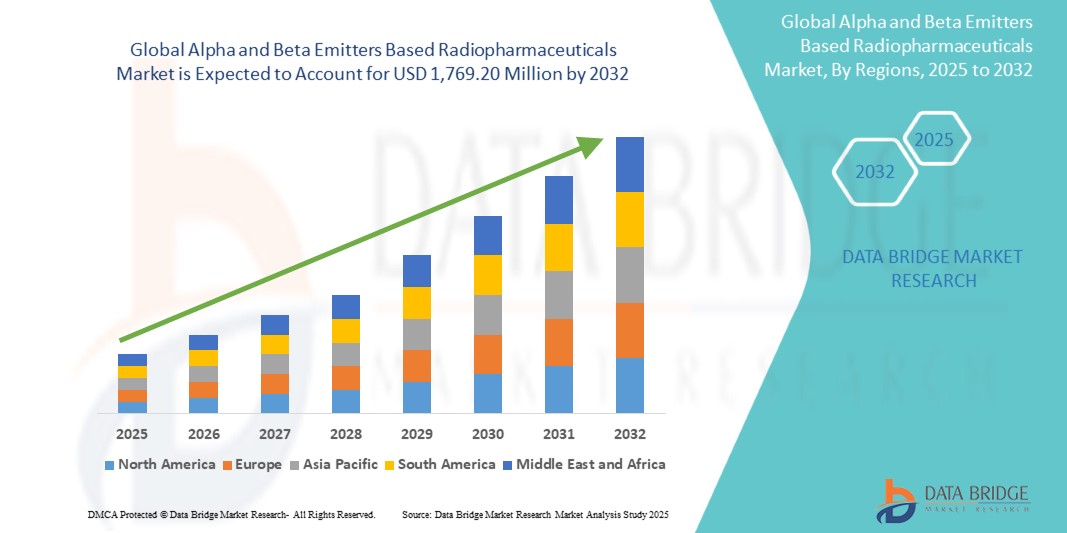
Expansion Rate of Alpha and Beta Emitters Based Radiopharmaceuticals Market
According to Data Bridge Market Research, the size of the global alpha and beta emitters based radiopharmaceuticals market was expected to be USD 801.45 million in 2024 and is projected to grow at a compound annual growth rate (CAGR) of 10.4% to reach USD 1,769.20 million by 2032.
Read More: https://www.databridgemarketresearch.com/reports/global-alpha-and-beta-emitters-based-radiopharmaceuticals-market
Conclusion
Alpha and beta emitters in radiopharmaceuticals represent powerful tools in the fight against cancer and other diseases. Alpha emitters offer high precision and potent cell-killing ability for targeting microscopic disease, while beta emitters provide effective treatment for larger tumor burdens with well-established clinical applications. Despite challenges related to production, safety, and dosing, ongoing advances in targeting, isotope availability, and personalized medicine promise to expand their therapeutic impact.
Note: IndiBlogHub features both user-submitted and editorial content. We do not verify third-party contributions. Read our Disclaimer and Privacy Policyfor details.







